Feeding Intolerance & Problem Solving
When your child first starts tube feeding, it may take a few days for their body to adjust to the formula and feeding routine. But there are times when he or she simply may not tolerate the feeding formula you have been asked to use – your child may feel unwell and cannot take all of the formula each day. This can become a problem if your child is not able to get the nutrition and water needed, or if your child is having unpleasant symptoms that makes him or her feel unwell.
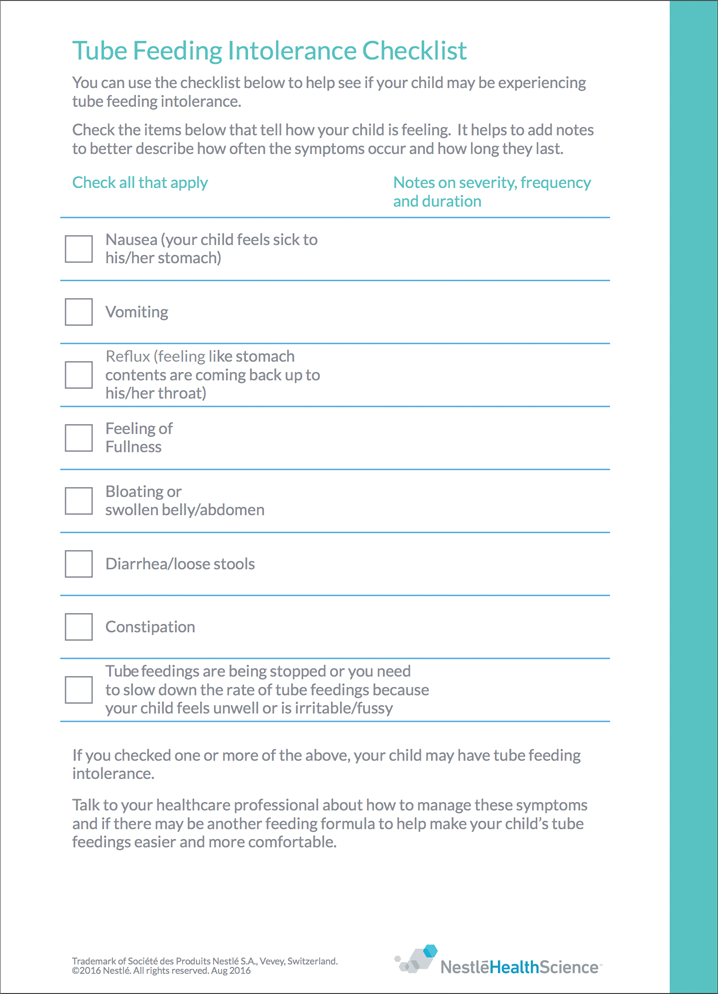
Feeding intolerance is often talked about by the signs or symptoms children have – which may vary from feeling full and having a swollen belly (abdomen) to vomiting or diarrhea. Being on a tube feeding does not mean that your child should feel uncomfortable during or after taking their formula.
You can use this checklist to help see if your child may be experiencing tube feeding intolerance.
→CLICK HERE TO VIEW/DOWNLOAD THE CHECKLIST