Tube feeding is a way of getting liquid nutrition through a tube.
Your child may need a tube feeding if he or she:
- Cannot get enough nutrition by eating or drinking by mouth; or
- Has difficulty chewing or swallowing easily or safely
To help make sure your child gets the nutrition and fluids he or she needs, your healthcare professional may suggest a tube feeding, either on its own or added to your child’s daily food and drink intake.
Tube feeding can help your child grow and develop. It is another way for your child to get the nutrition they need. With a feeding tube in place, your child can still take part in family activities like mealtimes. Having the support of your family and friends may make your child’s home tube feeding a more comfortable experience.
It is common for parents to have many questions about tube feeding, but once they see the benefits, many wish they had started sooner.
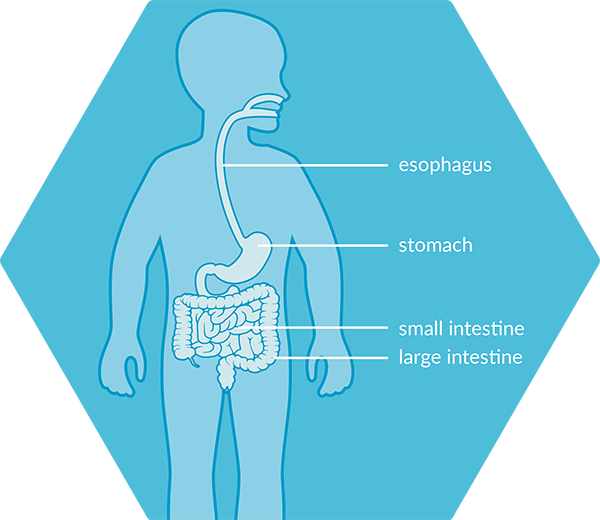
There are different locations and routes through which a feeding tube can be placed.
“
You can actually feed anywhere, anytime"
Suzanne, Nathan’s mum
→CLICK HERE TO WATCH THE FULL VIDEO IN OUR REAL STORIES SECTION
Below is a brief summary of the different tube feeding routes:
Tube feeding through the nose
NASOGASTRIC OR ‘NG-TUBE’:
The feeding tube goes through the nose, down the esophagus or food tube, and ends in the stomach.
NASOJEJUNAL OR ‘NJ-TUBE’:
The feeding tube goes through the nose, down the esophagus or food tube, continues through the stomach, and ends in the small intestine.
Tube feeding through the stomach
GASTROSTOMY OR ‘G-TUBE’:
The feeding tube goes through a small opening in the skin directly into the stomach.
JEJUNOSTOMY OR ‘J-TUBE’:
The feeding tube goes through a small opening in the skin into the jejunum or small intestine.
Tube feeding can be a safe and reliable form of feeding that allows you to track the amount of food and liquids your child is receiving.
“
It’s much tidier than people think"
Mariam, Yehoshua’s mum
→Click on this link to watch the full video in our real stories section
There are different ways to deliver tube feedings and different types of feeding schedules, depending upon what your healthcare professional has prescribed for your child.
Nutrition can be delivered continuously or given at meal times with breaks during the day (intermittent nutrition).
Continuous nutrition can be done by gravity or using a pump.
-
By gravity: A bag filled with formula or the pack of the formula hangs above the child to let the formula drip down into the tube and then into stomach. Roller clamps can be used to control the rate of flow.
-
Pump Feeding: A feeding pump can be programmed to run at whatever times and feeding rates required to deliver feedings. Make sure your healthcare professional demonstrates how to use the pump before you go home.
Intermittent nutrition can be done by gravity, using a pump or using a syringe.
-
Intermittent feeding is a type of tube feeding that provides a certain amount of formula over a short amount of time (usually 30-60 minutes), and is typically provided several times per day.
-
With a syringe: formula is poured into the syringe, then the plunger is used to push the food directly into the feeding tube.
It may be difficult to understand at first, but as you gain more experience, tube feeding can and will become easier. Even though your child is being tube fed, being included in family mealtimes and social events that involve food is just as important for your child as it is for you and your family. Speaking about tube feeding with your child will help alleviate any confusion and will allow your child to feel more reassured and comfortable during mealtimes.
There is also a wide range of formulas for your healthcare professional to choose from.
Formulas are developed to meet a child’s specific needs, including energy content, fibre content, as well as vitamin and mineral content.
Click on the Types Of Formulas section to better understand the different types of formulas available.
As you continue to tube feed your child at home, it’s natural to have questions, or to need some help. Your child's healthcare team can help you answer questions such as:
- What can I expect from the tube feeding experience and the different tube feeding options available?
- What type of equipment is needed and how do I set it up?
- How do I know if my child is getting enough nutrition?
- How do I know my child is having feeding intolerance?
Mealtime is an important opportunity for socializing, and a part of life that children should be involved in and enjoy from an early age. Even though your child is being tube fed, being included in family mealtime and social events that involve food is just as important for your child as it is for you and your family. Work with your healthcare professional to find a feeding schedule that works for you and your family.
For more information on tube feeding instructions, formulas, and more, visit:
mytubefeeding.ca
→CLICK HERE TO BETTER UNDERSTAND THE DIFFERENT TYPES OF FORMULAS AVAILABLE FOR FEEDING